Sometimes labour doesn’t go as planned and your baby will need help to be born. Help can involve relatively simple procedures like breaking the membranes (waters), to more medically demanding procedures such as caesarean section.
While some women have a preference for assisted births, others prefer to have no interventions at all. From a medical perspective, interventions are only introduced when they are necessary for the health of the mother or the baby.
On this page:
- Induction of labour
- Forceps birth
- Vacuum birth
- Episiotomy
A) Induction of labour
Approximately one-quarter of women have an induction of labour. The most common reasons are:
- Health concerns, such as diabetes or high blood pressure
- The health of your baby
- The pregnancy has gone more than 10 to 12 days beyond the due date and there is a risk that the placenta can no longer sustain the baby’s life
- Your waters have already broken, but you are not having contractions.
- You will only be offered an induction if your health or your baby’s health is at risk.
When your doctor recommends an induction you can expect that they will explain:
Why it is a good idea for you to be induced
- The possible risks to your health or your pregnancy if you wait for labour to start naturally
- The possible risks if you have an induction
- How they plan to induce your baby.
- If they don’t explain, use this list to ask them questions.
Some women will choose to ‘wait and see’ if labour will start on its own. It’s important that you consider all the risks and benefits in your particular situation so that you are able to make a well-informed decision.
Risks with induction
While not having an induction can put the health and even the life of your baby at risk, there are also risks with having an induction.
Having an induction for reasons other than prolonged pregnancy may increase the chance that you will need an emergency caesarean section.
Women who are induced are more likely to experience above-average blood loss after the birth.
How is labour induced?
First, the doctor or midwife will do an examination of your cervix. The examination takes only a few minutes but it can be a little uncomfortable. Based on this examination your doctor or midwife will recommend one of the following methods of induction:
- Artificially breaking the waters (the membranes or the sac around your baby)
- Artificially breaking the waters and oxytocin
- Prostaglandin
- Cervical ripening balloon catheter.
- An induction might involve one or several of these methods.
1) Breaking your waters
If your waters have not broken, the doctor can do this for you. The procedure is called Artificial Rupture of Membranes or ARM. The doctor makes a hole in your membrane sac to release the fluid inside.
This procedure is done through your vagina using a small instrument. Sometimes releasing the waters is enough to get things going and labour will start. However, most women will also need oxytocin. Things to know
The vaginal examination needed to perform this procedure may cause you some discomfort.
Although ARM is usually straightforward, it can increase the risk of cord prolapse, bleeding and infection
2) Oxytocin
Oxytocin is the hormone that causes contractions. A synthetic version can be given if your waters have broken but contractions don’t start. Oxytocin is given through a drip in your arm. Once contractions begin, the rate of the drip is adjusted so that contractions occur regularly until your baby is born. This process can take several hours. Your baby’s heart rate will be monitored throughout labour using a CTG machine.
Things to know
It will be hard to move around because you are attached to a drip and the CTG monitor. While you can stand up or sit down, it will not be possible to have a bath or move from room to room.
Sometimes oxytocin can cause the uterus to contract too frequently, which may affect the pattern of your baby’s heartbeat. If this happens you will be asked to lie on your left side and the drip will be slowed to reduce the number and strength of your contractions. Another drug may be given to cancel the effect of the oxytocin.
3) Prostaglandin
Prostaglandin is a hormone that prepares your body for labour. A synthetic version can be inserted into your vagina, either in the form of a gel or a pessary. When the prostaglandin is in place, it’s a good idea to lie down and rest for at least 30 minutes. Once the prostaglandin has been inserted you will need to remain in hospital.
When the prostaglandin takes effect, your cervix will soften and open. If you have the gel, you may need one, two, or three doses (given every six to eight hours). The pessary slowly releases the prostaglandin over 12 to 24 hours. When the cervix is soft and open, your body is prepared for labour. The next steps will vary from woman to woman – some might need an ARM to break their waters, and some women might need oxytocin to stimulate the contractions.
Things to know
Prostaglandin sometimes makes your vagina sore. However, there is no evidence to suggest that your labour will be any more painful than a labour that has started naturally.
A few women will react to the prostaglandin and have nausea, vomiting or diarrhoea, but this is rare.
Very occasionally prostaglandin can cause the uterus to contract too much, which may affect the pattern of your baby’s heartbeat. If this happens you will be asked to lie on your left side. You may be given a medication to relax the uterus. If you have a pessary this may need to be removed.
4) Cervical ripening balloon catheter
Your doctor may recommend using a cervical ripening balloon catheter over prostaglandin. This is a thin tube or catheter with balloons on the end. The catheter is inserted into your cervix and the balloons are inflated with saline. Once inflated the balloons apply pressure to the cervix. The pressure should soften and open your cervix.
When the catheter is in place, you will need to stay in hospital but you can move around normally. Fifteen hours after the catheter has been inserted or when it falls out, you will be re-examined. During this time the nurses will periodically check you and listen to your baby’s heart.
What happens next will vary from woman to woman – some might need an ARM to break their waters. Some women might need oxytocin to stimulate the contractions.
Things to know
The vaginal examination needed to perform this procedure may cause you some discomfort.
B) Forceps birth
Forceps are used to help the baby out of the vagina. They may be used if you are too exhausted to push, the baby is in an awkward position or there are concerns for your baby’s wellbeing. Sometimes the forceps leave a mark on the baby’s cheeks, but these soon fade. You will usually need an episiotomy.
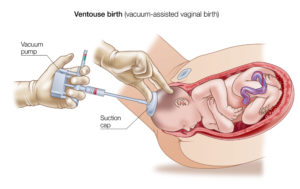
C) Vacuum birth
This is more commonly used in labour than forceps. The vacuum cup is made of plastic and is attached to a suction device. The cup is inserted into the vagina and creates a vacuum against the baby’s head. This helps the doctor to gently pull the baby out. It may cause a raised bruise on the baby’s head, but this soon fades, usually within a day. You may need an episiotomy.
D) Episiotomy
An episiotomy is a cut made in the perineum (the tissue between the vagina and the anus). Sometimes it is necessary to make the opening to the vagina bigger, especially if you need a forceps birth or if the baby is distressed. A local anaesthetic is used to numb the area and you will need stitches afterwards. The stitches will dissolve by themselves.
Which is better?
Your doctor will explain why she thinks you need an assisted birth, and what your options are. She’ll observe your bump and examine you internally, to check your baby’s position and make sure an assisted birth is the right thing to offer you. She’ll then decide which instrument to use and talk this through with you. All options have pros and cons and will be weighed by your doctor in charge.
If your doctor thinks that an assisted birth is possible, but could be difficult, you’ll be moved to an operating theatre. This is in case a caesarean is needed. Assisted birth is less likely to be successful if:
- Your body mass index (BMI) is over 30
- Your baby weighs more than 4kg
- Your baby is lying back-to-back
- Your baby’s head isn’t low down in your birth canal
How can I help myself to recover from an assisted birth?
Postnatal wards are busy places. Don’t be afraid to press your alarm while you’re on the ward if you’re in pain. The nurses should give you regular pain relief to ease the pain in your perineum and any soreness caused by your stitches. Paracetamol or anti-inflammatory drugs are the usual options.
Change your maternity pad often and wash your hands before and after you do this. Have a daily bath or shower to keep your stitches clean. Let your nurse or doctor know at the first sign of infection, such as a bad smell from your wound or if you are having problems when you wee.
Once you’re home, you may find it more comfortable to lie on your side or sit on a doughnut shaped cushion to relieve pain and pressure.
When you wee, you may find that your cut stings. Pour a jug of warm water over the area while you wee. This will dilute your wee, reduce the sting, and keep your perineal area clean.
Squatting on the toilet, rather than sitting, may also help to reduce the stinging. But if it’s very uncomfortable, bathing or washing your wound afterwards in warm water may help to ease the discomfort.
It’s natural to feel anxious about having a poo if you have stitches for an episiotomy or tear. If it was a severe tear, your midwife or doctor may prescribe a laxative to help things along. The laxative will be very gentle, so there’s no need to worry that you’ll be caught out by the urge to go to the toilet.
To avoid constipation, drink between one litre and three litres of fluids a day and have a good level of fibre in your diet. Try to get up and about to help your bowels move. Go to the loo as soon as you feel the urge, and don’t be rushed.
If you are finding it hard to control your wee, practising your pelvic floor exercises will help.
If you are still having problems with incontinence several weeks after giving birth, talk to your doctor.
If you need advice assisted births, please feel free to schedule an appointment to see Dr. Gan.
— Dr.Gan Kam Ling
Consultant Obstetrician And Gynaecology



Add a Comment