Fertility – The scale of the problem
A normal fertile couple in their mid-20s having regular sex has a one in four chance of conceiving each month. This means that around nine out of ten couples trying for a baby will conceive within a year. However, one in ten will not – and these couples are either subfertile or infertile. (In this booklet, as in everyday life, the term ‘infertility’ will be used to describe both). Infertility is usually defined by doctors as the inability to conceive after at least one year of trying. However, many ‘infertile’ couples can be helped by assisted-conception treatments.
Before couples embark on assisted conception there are other investigations and treatments which might also help; furthermore, many patients once enrolled in infertility programmes find they do become pregnant naturally, despite many years of trying.
Assessing the causes
Investigations carried out by a family doctor or specialist clinic can provide the likely cause of infertility in most cases. Only around 20 per cent remain unexplained – and even then treatment can be successful. The female partner is responsible for a couple’s infertility in around 40 per cent of cases, and the male partner in a further 40 per cent. The tests required to determine a specific cause will assess ovulation, the quality of the fallopian tubes, and hormone levels in women; and sperm production (numbers, movement and shape) in men.
Male infertility: the causes
- Low sperm count; normally, men produce at least 20 million sperms per milliliter of semen (that’s around one sixth of the total ejaculate); fewer is judged to be subfertile.
- Poor sperm motility; sperms will then be unable to swim through the cervix to meet the egg in the fallopian tube
- Poor shape (known as ‘morphology% so that an individual sperm is unable to penetrate the outer layer of an egg
- Non-production of sperm (because of testicular failure) or complete absence of sperm (perhaps because of an obstruction)
- Coital difficulties; perhaps because of ejaculatory failure or impotence
Female infertility: the causes
- Hormonal disorders; as a result, egg follicles might not grow within the ovary, or an egg might not be released (ovulation)
- Damaged or blocked fallopian tubes, which will prevent an egg and sperm meeting
- Endometriosis, in which womb tissue invades and damages neighbouring reproductive tissue
- Excessively thick cervical mucus, which prevents sperm—passing through
- Assisted conception may help most (though not all) of thes conditions, and there is evidence that repeated cycles treatment can restore fertility to near normal levels.
Assisted conception is not usually a first resort in the treatment of infertility. Other options such as advice on the timing of intercourse may have been tried first. In fact, the treatment route which a doctor chooses will mainly depend on the result of investigations. For example, fertility drugs with timed intercourse will be no help to a couple whose infertility is a result of the female’s blocked fallopian tubes; only surgical repair or assisted conception will help in this case.
The range of options is wide, and will depend on the diagnosis and type of infertility discovered. Thus, the decisions which patients and doctors must make are considerable. However if assisted conception is thought appropriate, the procedures available are ovulation induction (with fertility drugs), in vitro fertilization (IVF), gamete intrafallopian transfer (GIFT), artificial insemination by donor (AID or DI), intrauterine insemination with or without super ovulation (IUD, egg donation and IVF, and intracytoplasmic sperm injection (ICSI) with IVF.
Ovulation induction
The principle of ovulation induction is to stimulate the ovaries (with fertility drugs) to produce a small number of eggs (usually two and no more than three), and to allow fertilization to occur by natural intercourse. Women most suited to this form of treatment are those with hormonal disorders and a condition known as polycystic ovary syndrome. Crucial for success is that intercourse is timed to coincide with the ovulation which treatment has achieved. Monitoring of the response to treatment is therefore a vital part of the programme, to maximize the chance of a successful pregnancy and minimize any risks. The average chance of conception after one cycle of treatment ranges from 15 to 25 per cent.

Prof. Edward – Pioneer of “test tube baby’
In Vitro Fertilization
IVF is the original ‘test-tube baby’ technique, and probably the most widely practiced assisted-conception procedure in the world. In simple terms, IVF removes several eggs from the ovary, fertilizes them in the laboratory with sperm from the male partner and transfers a small selection of the resulting embryos to the womb for implantation and pregnancy. Although IVF was developed to treat couples whose principal cause of infertility is tubal damage, the technique has also been found useful in those with endometriosis, sperm disorders (poor sperm counts or morphology) and even unexplained infertility. Studies indicate that the expectation of pregnancy from one cycle of treatment is around average 25 per cent in younger women (mid-20’s). However the pregnancy rate can go as high as 40% or even more (depending on condition of the women and IVF centre) and the chance of delivery slightly less. Overall, the average take-home baby rate from IVF is about 15 per cent for each cycle of treatment. These rates are not much different from those of normal fertile couples. Most studies have shown pregnancy rates falling in women after the age of 35, which is why many infertility specialists encourage couples to act quickly when the female partner is already in her early thirties.
Step by step in IVF
- Drug treatment, to stimulate several eggs to mature
– GnRH agonist to suppress all other hormone activity (injections/nasal spray for (usually) two weeks before gonadotropins and then a further 10 — 14 days depending on response)
– Alternatively GnRH antagonist can be used to suppress all other hormones (as in agonist). However, this is started after the use of gonadotropins. The overall cycle length is reduced by 2 weeks by using GnRH antagonist
– Gonadotropins to stimulate the growth of follicles and cause ovulation
- Monitoring of treatment, to measure the growth of follicles, individualize drug doses and prevent serious side effects
– By transvaginal ultrasound scanning (two or three times during a treatment cycle) Sometimes by measuring hormones in a blood sample
- Egg collection, usually under local anaesthetic, lasts between 10 and 20 minutes
– Guided by transvaginal ultrasound Collected through the vagina (32-36 hours after final hormone injection)
- Sperm sample,provided on the same day as egg collection
- Fertilization
– Eggs and sperm prepared and cultured together overnight
– Eggs examined next day under microscope
- Embryo transfer (usually two or three days after fertilization)
– Transvaginal transfer of no more than three embryos
– Embryos placed in the womb
– Spare embryos usually frozen
- Pregnancy testing/monitoring
Gamete intrafallopian transfer
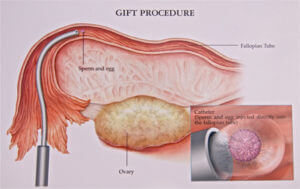
GIFT differs from IVF because the eggs collected from the ovary are transferred back to the fallopian tube almost immediately after collection (together with a small sample of sperm). Doctors just have time to examine the eggs, select no more than three and add sperm before placing the mixture back into the tube. So, unlike IVF, fertilization does not take place in vitro (i.e. in the laboratory) but in its natural environment in the fallopian tube. However, because eggs are collected and replaced during the same procedure, doctors have to see what’s going on – and this is done with a minor surgical instrument known as a laparoscope. Laparoscope use requires a small incision in the abdomen – and also requires a general anaesthetic.
GIFT, like IVF, is a proven and successful assisted- conception technique and because it requires no laboratory fertilization or examination of embryos, can often be performed in a local hospital as well as in a specialist clinic. However, because fertilization takes place within the fallopian tube, it is essential that the female partner has healthy tubes.
Pregnancy rates for GIFT will depend on individual circumstances but have been reported as high as 36 per cent per treatment cycle, and average live birth rates at 26 per cent. While some clinics might achieve these very high success rates, others will have far less successful results. GIFT has also proven to be a useful treatment for couples with unexplained infertility and in mild cases of endometriosis, provided the fallopian tubes are healthy! Drug treatment and monitoring in GIFT are identical to IVF as far as Step 3 in the Step-by-Step in IVF above.
Artificial insemination
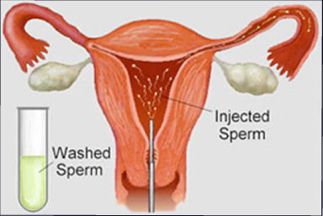
The most recent studies of artificial insemination suggest that the best results are achieved when insemination coincides with ovulation induced by fertility drugs, as in IVF and GIFT. However, it is important that doctors undertaking this ovarian stimulation monitor their drug treatment to ensure there are not too many follicles developing in the ovary. A lot of follicles will produce too many eggs and increase the risk of multiple pregnancy -so the usual aim is to generate no more than three eggs. This is far fewer than for IVF or GIFT, but ensures that the risks of multiple pregnancy are minimized. The early stages of treatment are therefore similar to Steps 1-2 in IVF. Only at the time of ovulation does the procedure change.
Then around the time of ovulation, a sample of sperm from the male partner is prepared and placed either in the cervix or high in the uterus of the female partner through a fine catheter. This latter procedure is known as intrauterine insemination, or IUI, as illustrated. Because fertilisation takes place in the natural environment (i.e. in the fallopian tube), the female partner’s tubes must be open.
The success rates from 1U1 following ovarian stimulation (super ovulation) are between 10 and 15 per cent per cycle but can reach 50 per cent after several attempts in one year. It is important that the male partner’s sperm count is within normal limits and the female’s tubes are healthy. Doctors might try four cycles of IUI and if these are not successful, then recommend other methods like IVF or GIFT.
In cases where the male partner has severe sperm disorders, frozen sperm from any anonymous donor may be used – this is known as donor insemination, or DI. All sperm donors must be screened for genetic disease and viruses. Recent breakthroughs in sperm injection techniques, like ICSI, mean that anonymous sperm donation is less frequently used.
Then, around the time of ovulation, a sample of sperm from the male partner is prepared and placed either in the cervix or high in the uterus of the female partner through a fine catheter. This latter procedure is known as intrauterine insemination, or IUI, as illustrated. Because fertilization takes place in the natural environment (i.e. in the fallopian tube), the female partner’s tubes must be open.
Step by step in IUI
- Drug treatment, to encourage two or three eggs to mature – Usually gonadotropins to stimulate the growth of follicles and cause ovulation
- Monitoring of treatment, to measure the growth of follicles, individualize drug doses, and prevent serious side effects – By transvaginal ultrasound scanning (two or three times during a treatment cycle) – Sometimes by measuring hormones in a blood sample
- Sperm sample, provided on the morning of ovulation, is prepared and inserted later that day
- Pregnancy testing, monitoring
Egg Donation
Egg (oocyte) donation is a treatment which may raise ethical issues and counseling is always important. The treatment was designed for women who were unable to produce eggs of their own. Egg donation is also appropriate for women with genetic disease, who might pass on a disorder to their children.
As many studies have illustrated, the key to success in egg donation is not so much the age of the recipient but the age of the egg donor. Eggs from women under 35 have been proven to be much more amenable to fertilization and pregnancy.
Egg donation is not a simple procedure. Egg donors require the same drug treatment and monitoring prior to egg collection as women undergoing IVF or GIFT. For these reasons, most egg donors tend to be young women (under 35) who are prepared to make such sacrifices of time and discomfort. Sometimes, they are relatives and close friends. All potential donors and volunteers must be screened for genetic diseases and viruses.
While the egg donor is in her collection, the recipient must be made ready for pregnancy – and this is also done by the usage of hormones. In fact, she is given two female hormones -estrogen and programme – to mimic a normal ‘pregnant’ cycle, in which the lining of the uterus (endometrium) thickens for implantation of the fertilized egg.
Step by step in egg donation
Donor
- Drug treatment, to encourage several eggs to mature GnRH agonist to suppress all other hormone activity (injections/nasal spray for (usually) two weeks before gonadotropins and then a further 10-14 days depending on response) – Alternatively GnRH antagonist can be used to suppress all other hormones (as in agonist). However, this is started after the use of gonadotropins. The overall cycle length is reduced by 2 weeks by using GnRH antagonist Gonadotropins to stimulate the growth of follicles and cause ovulation
- Monitoring of treatment, to measure the growth of follicles, individualize drug doses and prevent serious side effects – By transvaginal ultrasound scanning (two or three times during a treatment cycle) – Sometimes by measuring hormones in a blood sample
- Egg collection, usually under local anaesthetic – Guided by transvaginal ultrasound – Collected through the vagina (32-36 hours after final hormone injection)
- In vitro fertilization with sperm of recipient’s male partner
Recipient
- Previous investigations: no ovulation
- Hormone replacement therapy several days before transfer to prepare uterus
- Embryo transfer (usually two days after fertilization) – Transvaginal transfer of no more than three embryos – Embryos placed in the womb – Spare embryos usually frozen
- Pregnancy testing/monitoring
Once the eggs are collected from the donor, they are fertilized with a prepared sperm sample from the recipient’s male partner. Up to three embryos are transferred to the uterus of the recipient two or three days after fertilization; the rest are usually stored for later use.
Egg donation has been proven to be a successful assisted-conception technique and is the only treatment for women who are unable to produce eggs. Despite its success, its use remains limited, mainly because of a shortage of egg donors.
Fertilization by ICSI

The techniques of intracytoplasmic sperm injection, or ICSI, have been hailed as a revolution in the past few years and have finally offered a viable treatment for even the most difficult cases of male infertility. Where in the past doctors could offer nothing but adoption or DI to those couples whose infertility was a result of severe sperm defects, now ICSI appears to offer a real treatment solution.
the egg with a needle which
The ICSI technique makes use of the most powerful microscopes and ‘micromanipulators’; embryologists, for example, holding a single human egg at the end of a fine suction pipette, can penetrate is seven or more times finer than the diameter of a human hair. In normal conception, a single ejaculation of semen might contain more than 200 million viable sperms – but from this vast number only a few hundred will actually reach the released egg in the fallopian tube and be able to fertilize it. Men with total sperm counts below 20 million or so (or 5 million per milliliter) were always thought impossible to treat; now, ICSI can achieve fertilization with just one sperm cell injected into an egg.
In centres, where ICSI has been most successfully applied, as many as 70 per cent of eggs injected by this method are fertilized. This was often with sperm cells salvaged from samples which appeared to contain hardly any viable specimens. When eggs fertilized by ICSI were transferred to the female partner, pregnancy and take-home-baby rates were as high as in routine IVF (and in some cases higher!).
These microtechniques have now been developed to treat the infertility of men who not only produce poor-quality sperm, but those who produce no sperm at all because of blockage or other testicular disorders. A technique known as microepididymal sperm aspiration (MESA) actually removes a small specimen of semen from the epididymis and uses sperm cells retrieved for fertilization by ICSI. A similar technique, in which sperm cells are extracted from a tiny biopsy of testicular tissue (known as TESE), helps men who are unable to produce their own sperm. Results from both techniques have been most encouraging, suggesting that men who for various reasons are unable to ejaculate or generate sperm are now able to supply the sperm to fertilize their partner’s eggs.
Infertile couples who are recruited to ICSI treatment programmes will usually be carefully selected (severe sperm defects, for example) and will often have a record of failed IVF. Because there is a theoretical risk that the male partner’s infertility is the result of an inherited disease, counselling and genetic screening may be required. Most centres also require follow-up during and after pregnancy.
The female partner, of course, must undergo the routine procedure of superovulation and egg collection, while the male partner must produce a sperm sample (unless MESA or TESE are indicated). Crucial to the success of ICSI is the preparation and selection of sperm cells, which is done by a process of washing and grading. Sperm preparation allows just a few viable sperms to be salvaged from an otherwise unusable sample.
Step by step in ICSI
- Drug treatment, to stimulate several eggs to mature
– GnRH agonist to suppress all other hormone activity (injections/nasal spray for (usually) two weeks before gonadotropins and then a further 10 — 14 days depending on response)
– Alternatively GnRH antagonist can be used to suppress all other hormones (as in agonist). However, this is started after the use of gonadotropins. The overall cycle length is reduced by 2 weeks by using GnRH antagonist
– Gonadotropins to stimulate the growth of follicles and cause ovulation
- Monitoring of treatment, to measure the growth of follicles, individualize drug doses and prevent serious side effects
– By transvaginal ultrasound scanning (two or three times during a treatment cycle)
– Sometimes by measuring hormones in a blood sample
- Egg collection, usually under local anaesthetic, lasts between 10 and 20 minutes
– Guided by transvaginal ultrasound
– Collected through the vagina (32-36 hours after final hormone injection) 4. Sperm sample, provided on the same day as egg collection. The sample can be obtained in a natural way or following aspiration from the epididymis (MESA) or extraction from the testis (TESE)
- Fertilization
– One single sperm cell is injected into a single egg cell
– Eggs are examined the next day under the microscope to see whether fertilization has occurred
- Embryo transfer (usually two or three days after fertilization)
– Transvaginal transfer of no more than three embryos
– Embryos placed in the womb
– Spare embryos usually frozen
- Pregnancy testing/monitoring
THE RISKS OF ASSISTED CONCEPTION
Because all assisted-conception methods offer an overall chance of a baby of around 15 to 20 per cent for each cycle of treatment, the biggest hazard for those embarking on treatment is disappointment. However, as studies show, the chances of pregnancy do increase with additional cycles and are comparable to nature.
There are few risks associated with the actual treatments themselves. GIFT requires general anaesthesia for laparoscopy to take place and this can – on very rare occasions – cause complications. Indeed, this is one reason why infertility specialists in some countries have preferred IVF to GIFT – not because the results are better but because a general anaesthetic is not required.
The most common ‘side effects’ of treatment are multiple pregnancies. These not only cause serious social complications (particularly as the babies begin to grow!) but are also associated with higher rates of pregnancy loss and lower birth weight babies. The most publicized `danger’ of assisted conception has been a condition known as ‘ovarian hyperstimulation syndrome’ (OHSS), which can very rarely occur as a result of the drug treatment given in the stages before egg collection. Too high a dose of drug can cause excessive stimulation of the ovaries, which can be noticed as pain the abdomen. It is to avoid this risk – as well risk of multiple pregnancies – that doctors monitor drug treatment and its effect on the ovary.
COUNSELLING
In most countries counselling will be provided for all couples undergoing assisted conception. For many who have reached the stage of assisted conception, the frustrations of childlessness have already imposed severe emotional strains, so the offer of guidance and help through this difficult period is usually appreciated.
In addition, assisted conception as a medical treatment imposes its own demands, which makes counselling even more essential. The passage through a cycle of treatment is not always easy and as the statistics show, success cannot be guaranteed. Even couples who achieve pregnancy might still experience the severe disappointment of pregnancy loss.
Some couples also find that the dilemmas raised by assisted conception are more easily resolved after discussion with a trained counsellor – what to do about spare frozen embryos, how to accept the genetic anonymity of egg donation, how to face treatment failure ?
THE REAL CHANCES OF SUCCESS ?
Because around four in five couples undergoing a single cycle of assisted-conception treatment do not have a baby, it’s easy to talk about failure. But the truth is that the overall success rates of assisted conception are about as good as in nature, and sometimes even better. Because the chances of success continue to increase with each cycle of treatment, 100 couples embarking on assisted-conception treatment will find their number declining substantially after several cycles. After four cycles of treatment this cumulative’ pregnancy rate may reach 50 per cent following IVF or GIFT per couple treated. However, conception is less likely in women over 40. The latest breakthroughs in treating male infertility by ICSI mean that men with sperm disorders now have much better chances of fathering children.



Add a Comment