About one in five women of reproductive age have small cysts on their ovaries. These will cause few problems to the majority of women, but some may be further troubled by accompanying symptoms and even infertility. The condition is then known as polycystic ovary syndrome and may require specialist treatment.
About one in five women have polycystic ovaries. This term describes the appearance of the ovaries when they are seen on an ultrasound scan. The polycystic ovary syndrome (PCOS) is the name given to a condition in which women with polycystic ovaries have one or more additional symptoms. So, not all women with polycystic ovaries have polycystic ovary syndrome, but most women with PCOS do have polycystic ovaries.
The diagnosis of PCOS has been made much easier in recent years by the availability of ultrasound scanning. Before this, only women with the most severe symptoms could be diagnosed with accuracy; today, the condition can be detected even when the problems are only mild.
Normal Ovaries
Women have two ovaries; they are located in the pelvis alongside the uterus (womb). Their main functions are to release eggs and produce hormones.
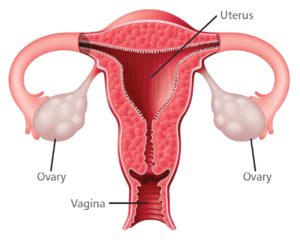
At birth, the ovaries are provided with thousands of eggs, each surrounded by cells which develop into a small, fluid-filled blister known as a follicle. Each month, in women with regular periods who are ovulating normally, one of these follicles will grow into about 20 millimetres in diameter and then release an egg (ovulation), which passes into the fallopian tubes. Here, fertilization takes place, before the fertilized egg (embryo) continues to the uterus to implant in the lining (endometrium) and develop as a pregnancy. If no egg fertilizes, the endometrium is shed as a menstrual period around 14 days after ovulation.
Three important groups of hormones- estrogens, androgens and progesterone — are also produced in the ovary. These in turn are regulated by the release of two further hormones from the pituitary gland at the base of the brain – follicle stimulating hormone (FSH) and luteinizing hormone (LH). These two ‘reproductive’ hormones influence the development of the follicle and the timing of ovulation.
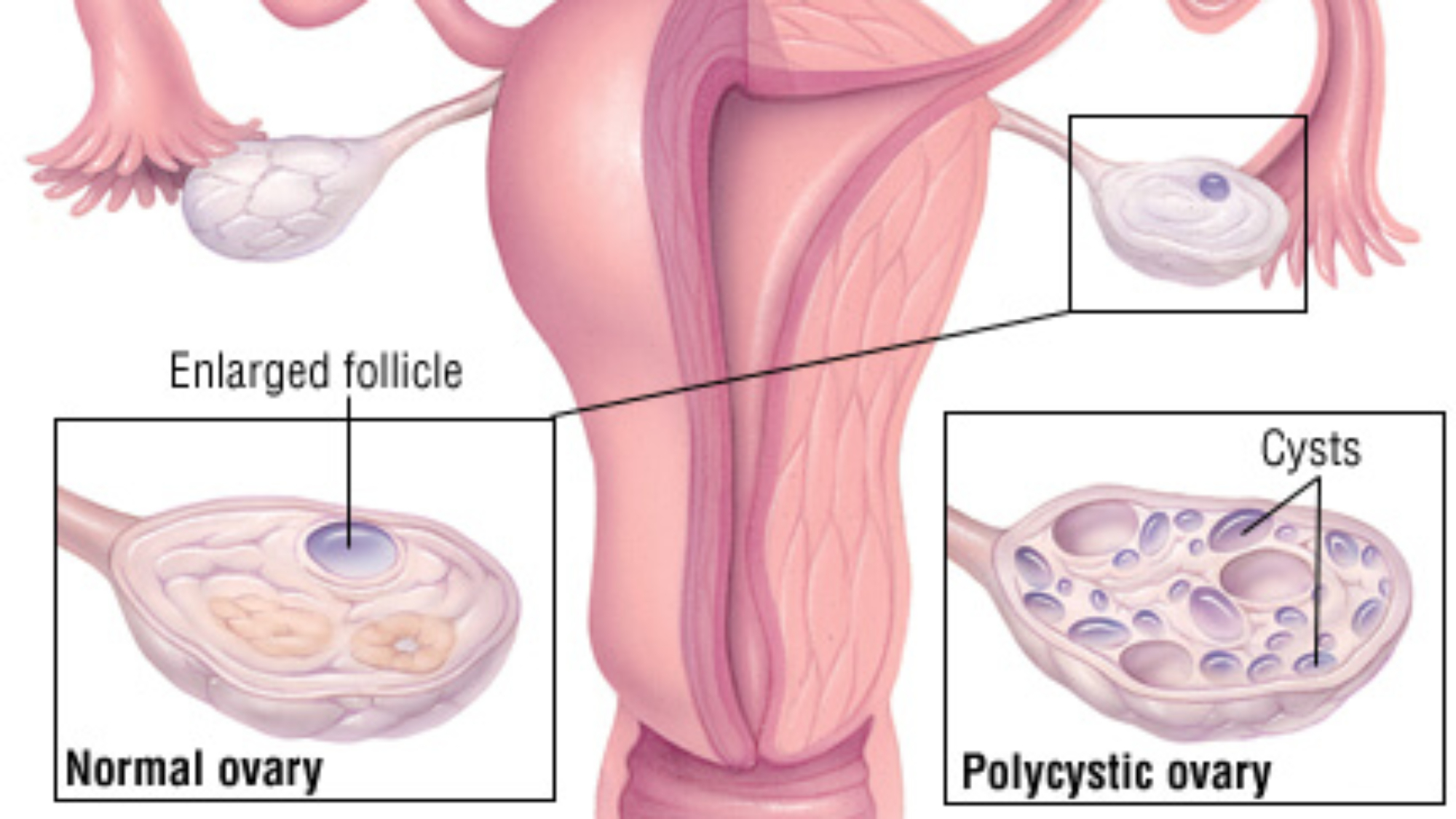
Polycystic Ovaries
Polycystic ovaries contain many small cysts — at least ten. Some of these cysts contain eggs, some are dormant, and others might secrete hormones. The cysts are quite small, usually no bigger than 8 millimeters, but they are clear enough on ultrasound to allow an accurate diagnosis. Blood tests might also reveal changes in hormone levels which are characteristic of polycystic ovaries, but these levels vary considerable from one woman to another.
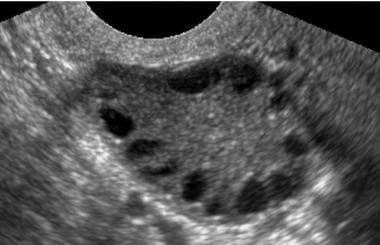
Transvaginal ultrasound scan of a polycystic ovary
Doctors are still not entirely clear why some women have polycystic ovaries. There may be a hereditary link, and they are present in women of all ages, many of whom show no symptoms of PCOS. In other words, ovaries do not suddenly become polycystic; but women who have always had polycystic ovaries may develop symptoms at any time.
The cause of polycystic ovaries is believed to involve an inability of the ovaries to produce hormones in correct proportions. The pituitary gland senses that the ovary is not working properly and in turn releases abnormal amounts of LH and FSH — which may mean that unusually high levels of LH are circulating in the bloodstream.
The Symptoms of PCOS
1. Menstrual Irregularities
The imbalance of hormone production from both the ovaries and pituitary may result in either irregular ovulation or no ovulation at all (known as `anovulation’). Menstrual periods may therefore become irregular- perhaps heavier than usual, perhaps occurring after long gaps (oligomenorrhoea) or perhaps not at all (amennorrhoea). Some women notice pelvic pain, which may be related to the effect of hormones on the flow of blood through the pelvic veins.
2. Fertility
Irregular ovulation usually means that pregnancy is more difficult to achieve; similarly, if ovulation is not taking place, it is just not possible to conceive without treatment. So, women with irregular cycles hoping to get pregnant will have a better chance once their monthly cycles have returned to normal.
3. Miscarriage
While miscarriage seems an unfortunate chance event for most couples, it is now known that women with PCOS who have high circulating levels of LH may be at greater risk. The explanation is probably that too high a level of LH in the bloodstream makes it more difficult for the egg to develop within the follicle, and for an embryo to implant within the uterus.
4. Skin problems
One of the hormones which may be released in usually high amounts from the ovary is testosterone, the ‘male’ sex hormone which circulates in both men and women. Excessive testosterone levels in women may be a cause of acne on the face and back, or unwanted hair on the face, chest, arms and legs. The levels of testosterone in women with PCOS are still much lower than those found in men.
5. Insulin Abnormalities and Obesity
Insulin abnormalities and obesity are common problems among women with PCOS. Obesity tends to be central (abdominal) in its distribution, and even lean women with PCOS may have a fat distribution favouring central omental and visceral fat.
PCOS is also associated with abnormal blood insulin levels, the hormone that regulates blood sugar levels. These abnormalities may include
– Hyperinsulinism (excess production of insulin)
– Insulin resistance (poor response of body tissues to insulin)
– Impaired glucose tolerance (a condition of borderline diabetes mellitus)
– Type 2 diabetes mellitus (non-insulin dependant diabetes)
Insulin resistance and hyperinsulinemia can occur in both normal-weight and overweight women with PCOS. By age 40, up to 35 percent of obese women with PCOS develop impaired glucose tolerance, and up to 10 percent of obese women with PCOS develop type 2 diabetes.
The everyday problems of PCOS are often only amenable to medical treatment, but there are also some lifestyle changes which can improve symptoms. For example, doctors know that the body’s hormone balance can be upset by excessive body weight, and certainly PCOS is more common in obese women than in those with a correct weight-to-height ratio. Equally, some women with polycystic
ovaries only develop symptoms when they put on weight. So, a correct weight-to-height ratio will help, and this can be measured by an equation called ‘the body mass index’ (BMI). Your BMI is your weight in kilograms divided by your height in meters and then squared — or as doctors would write, kg/m2. A normal BMI is between 20 and 25.
A danger to health?
The small cysts detected in polycystic ovaries do not get any bigger; in fact, they usually disappear only to be replaced by other similar cysts. They remain small (no bigger than 8 millimeters) and do not require removal by surgery. Sometimes, larger cysts (over 20 millimeters) might release an egg. Only very large cysts (over 50 millimeters) require surgery, and they can occur in any woman, whether she has polycystic ovaries or not. There is no link between the cysts of polycystic ovaries and ovarian cancer. However, although the risk is still very rare, women with few or absent periods are at an increased risk of endometrial cancer. This can happen when the womb lining (endometrium) becomes too thick; regular shedding in the form of a period prevents this. If the endometrium appears thick or irregular on an ultrasound scan, a D&C (dilatation and curettage) operation might be advised.
Obese women with polycystic ovaries are also at greater risk of heart disease — simply because excess weight is linked to high blood pressure and excessive levels of cholesterol in the bloodstream, both known risk factors for heart disease. A high fiber, low fat and low sugar diet at a young age, coupled with cessation of smoking may help reduce these risks in later life. Avoid “crash” diets and short-term weight loss. Sustain a long term sensible diet together with physical activity. Diabetes mellitus, is a condition, in which the body is unable to use sugar efficiently and is also associated with excess weight. Medication may he needed, however weight loss and a lower intake of carbohydrates will also help.
Indeed, being overweight is probably the cause of the greatest and most frequent problems for women with PODS.
Management of PCOS
It thus goes without saying that all women with polycystic ovaries should try to maintain a normal weight and to have regular periods. Medical treatment is usually confined to those with the troublesome symptoms of PCOS.
1. Menstrual irregularities
Irregular periods are a nuisance — as well as a suggestion of some hormonal disorder or risk of endometrial thickening. For women who have no wish to become pregnant, the contraceptive pill offers the easiest solution. This will produce a regular (though artificial) cycle and regular withdrawal bleeding during the Pill free week. Today, most gynaecologists would recommend a low dose variety for women with polycystic ovaries. Women, who cannot take the Pill might find improvement from a progestogen-only treatment, usually taken for 12 days every one to three months. This will induce bleeding, without any of the side effects associated with the estrogen in the Pill.
Any irregular bleeding while you are taking the Pill should be checked by a doctor. An ultrasound scan might be advisable; similarly, a routine cervical smear should be taken once every three years.
2. Difficulty in conceiving
While failure to ovulate is the usual reason for infertility in women with polycystic ovaries, it is also worthwhile ensuring that other important factors- like your own fallopian tubes or your partner’s semen – are also OK.
Monitoring ovulation. In normal cycles, ovulation takes place 14 days before a period starts – so only if your cycles is 28 days, ovulation will take place on day 14. If your cycles is 27 days, ovulation will be on day 13; likewise if it is 35 days, ovulation will be on day 21. These sums are important if you are timing sexual intercourse to coincide with ovulation. The most reliable way to predict ovulation is with an over-the-counter urinary test kit. This measures the surge of LH which occurs around the time of ovulation.
Testing should begin in a day or two before you expect to ovulate, while intercourse should take place the on the day the test shows a colour change, and on the day after. Temperature charts can indicate hormonal changes in the cycle but are not accurate predictors.
Ovulation can be monitored by ultrasound, but this of course requires visits to hospital and is thus usually reserved for women having more extensive treatments and those who have difficulties with the urine tests.
A blood test seven days after presumed ovulation allows doctors to measure the level of the hormone progesterone to check if ovulation did in fact take place.
Of course, most of this monitoring- whether simple or more complicated — is performed so that sexual intercourse might be more timed to coincide with ovulation. If you have regular cycles and are ovulating normally, intercourse two or three times a week should achieve a supply of sperm sufficient to fertilize the egg when it is released. Long periods of abstinence appear to worsen sperm function.
Many patients report that intensive monitoring can remove much of the spontaneity from their sex life. A short break from treatment — perhaps a month or two — might relieve the pressure and allow more relaxed love-making.
Drugs to induce ovulation
In cases where ovulation is irregular or non-existent, drugs can be used. The most common is clomiphene citrate, which is taken as a tablet for five days from the second day of menstruation. Results show that seven out of ten women given clomiphene do ovulate, but only about one in three actually become pregnant. The starting dose is usually 50 milligrams, which may be increased to 100 milligrams. Clomiphene can cause thickening of mucus in the cervix, so a post-coital test can tell doctors how well the sperms are surviving in the genital tract.
However, whilst clomiphene is a useful drug for many women with infertility problems, it is not always suitable for those with PCOS because it can cause an exaggerated rise in blood levels of LH which could impede fertilization or increase the chance of miscarriage. So, if clomiphene has not been successful in women with PCOS within six months, more investigations and alternative treatments are usually called for.
Side effects with clomiphene have been reported, notably stomach and bowel upsets, hot flushes, bloating, headache, dizziness, depression and breast discomfort. Multiple pregnancy is a risk whenever ovulation is induced with fertility drugs. In natural conception the risk is about one in eighty, in induced ovulation about one in twenty. There is no increased risk of birth defect from fertility drugs.
Further treatments If tablets fail. injectable hormones are used to stimulate the ovaries more directly. The most common injections involve a group of hormones known as gonadotropins.
The gonadotropin preparations are produced by means of modem biotechnological methods. These injections can be given by subcutaneous (under the skin) rather than by the deeper intramuscular injections. These products work adequately in women with PCOS. However. because the polycystic ovary contains many small cysts (which are. in effect follicles). the ovary is very sensitive to stimulation by these hormones. In view of this. courses of treatment begin with low doses. and the growth of the follicles is carefully monitored by ultrasound. These scans may be supported by measirements of estrogen release from the ovary into the bloodstream. If monitoring shows that too many follicles are developing and the risk of multiple pregnancy is high. doctors will usually suspend treatment and cancel that cycle.
A second gonadotropin — human chorionic gonadotropin hCG) — is given to stimulate release of the egg from the follicle. This preparation is given when the ovary contains one or more mature follicles. hCG takes between 36 and 40 hours to work — so if it is given in the morning, ovulation can be expected the following evening or night.
Women with PCOS given gonadotropins are at an increased risk of a rare but serious condition known as ovarian hyperstimulation syndrome — so careful monitoring is essential. The condition occurs if many follicles are stimulated and results in abdominal distension and nausea.
In vitro fertilisation (IVF)
IVF, the test-tube baby’ technique in which a woman’s eggs are fertilized with her partner’s sperm in the laboratory is usually recommended to women who have blocked fallopian tubes. or men with poor sperm. IVF is sometimes offered to women with PCOS who want to conceive when other treatments have failed. However. PCOS on its own is not an indication for IVF. Women with PCOS who undergo IVF are at greater risk of the ovarian hyperstimulation syndrome and must be carefully monitored.
Laparoscopic ovarian diathermy
This is a minimally-invasive operation performed through a laparoscope. The procedure actually burns parts of the ovary to correct any hormonal abnormalities and this make ovulation possible. While it has been used in recent years with apparently good results, it should be noted that it has potential side effects on its own like surgical complications. pelvic adhesions and anaesthetic risks.
3. Miscarriage
Miscarriage in women with PCOS is thought to be associated with raised levels of LH. However. it has not been shown to be preferable to suppress the release of LH before inducing ovulation – which can be done by using a drug known as gonadotropin releasing hormone analogue (GnRHa). GnRH analogues can be given as a daily injection or as a nasal spray. Once blood levels of LH have fallen, ovulation can be induced with FSH. Laparoscopic ovarian diathermy also results in a lowering of LH levels in the bloodstream and might also help reduce the risk of miscarriage.
4. Skin Problems
The usual therapies for acne and unwanted hair are a combination of estrogen (as found in the contraceptive pill) and an ‘anti-androgen’ hormone like cypoterone acetate. This therapy, of course, has a contraceptive effect – and so is of little use to those trying to conceive. There are alternative treatments without any native contraceptive effect, and these important issues should be discussed with your doctor.
Waxing and electrolysis can be helpful, especially while waiting for the hormonal treatments to work. However, they should only be performed by trained therapists, as scarring can result from unskilled treatment. If PCOS is diagnosed as the cause of the problem, correction of the hormonal abnormality is the logical solution.
5. Insulin Abnormalities and Obesity
Lifestyle modifications combining behavioural changes, diet and exercise is one of the simplest and most effective approaches to managing obesity, insulin abnormalities, menstrual irregularities, and other symptoms of PCOS.
Women with PCOS who are overweight should aim for a 5-10% weight loss with focus on abdominal fat loss (reduction in waist circumference) and fitness improvement. It has been shown in a number of studies that approximately 5% reduction in weight will restore ovulation and reduce miscarriage rates. A sensible diet of low fat, low sugar and high fibre should be observed. Other behavioural changes like smoking cessation and reduction in alcohol consumption will also help. It must be noted that lifestyle modification require a lot of support both from health care providers as well as the family
Insulin sensitizing drugs is an option for treating insulin abnormalities associated with PCOS. This class of drugs include Metformin (Glucophage) that is prescribed for the treatment of diabetes. Metformin also helps restore menstrual cycle and stimulates ovulation. It can be used on its own or in combination with clomiphene citrate.


Add a Comment